Province releases planning scenarios for COVID-19, prepares for 153,000 to 408,000 cases
They are not predictions or expectations, but the province has released three ‘what if’ scenarios to assess the potential impact of COVID-19 transmission on Saskatchewan’s health care system.
These scenarios plan for – but do not predict – anywhere between 153,000 and 408,000 cases, and anywhere between 3,075 and 8,370 deaths.
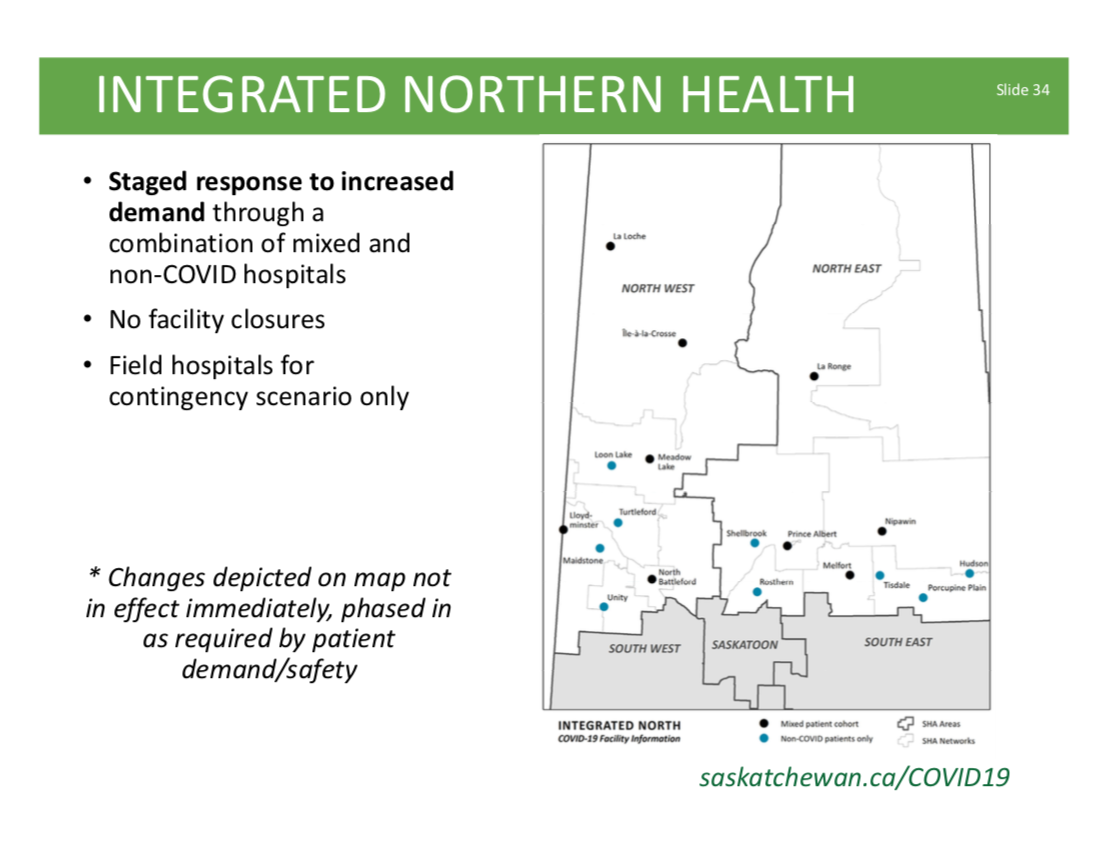
To show the different responses in ‘flattening the curve’, the Saskatchewan Health Authority (SHA) explained modelling for three separate response scenarios in a 45-page report.
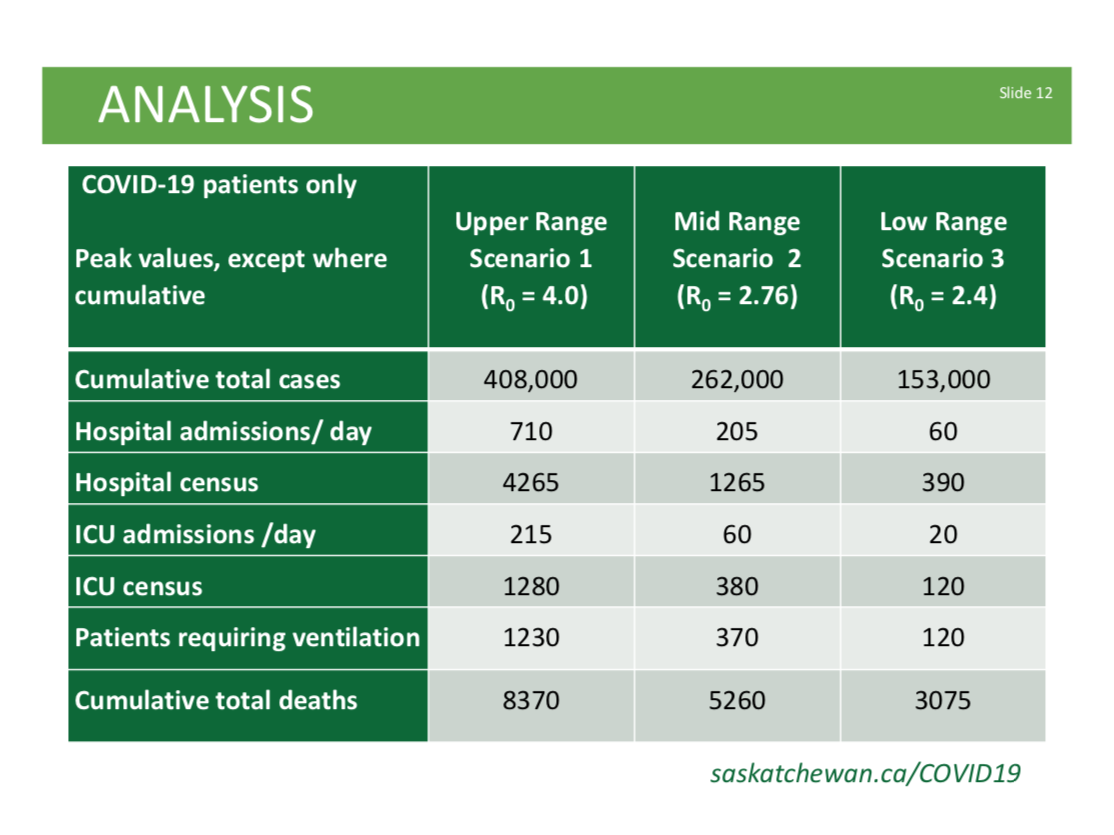 This chart was included in the province’s modelling scenarios. They are not a prediction or expectation of what’s to come in the COVID-19 pandemic. (submitted photo/SHA)
This chart was included in the province’s modelling scenarios. They are not a prediction or expectation of what’s to come in the COVID-19 pandemic. (submitted photo/SHA)